Derek, in more recent years, has played a key role supporting the development of PPI in University of Galway, contributing to programmes of research such as PPI Ignite @ University of Galway, the HRB-Trials Methodology Research Network and Evidence Synthesis Ireland.
In 2020, Derek was appointed as an Honorary Professor at University of Galway for his contribution to the growing recognition of University of Galway as a leader in PPI.
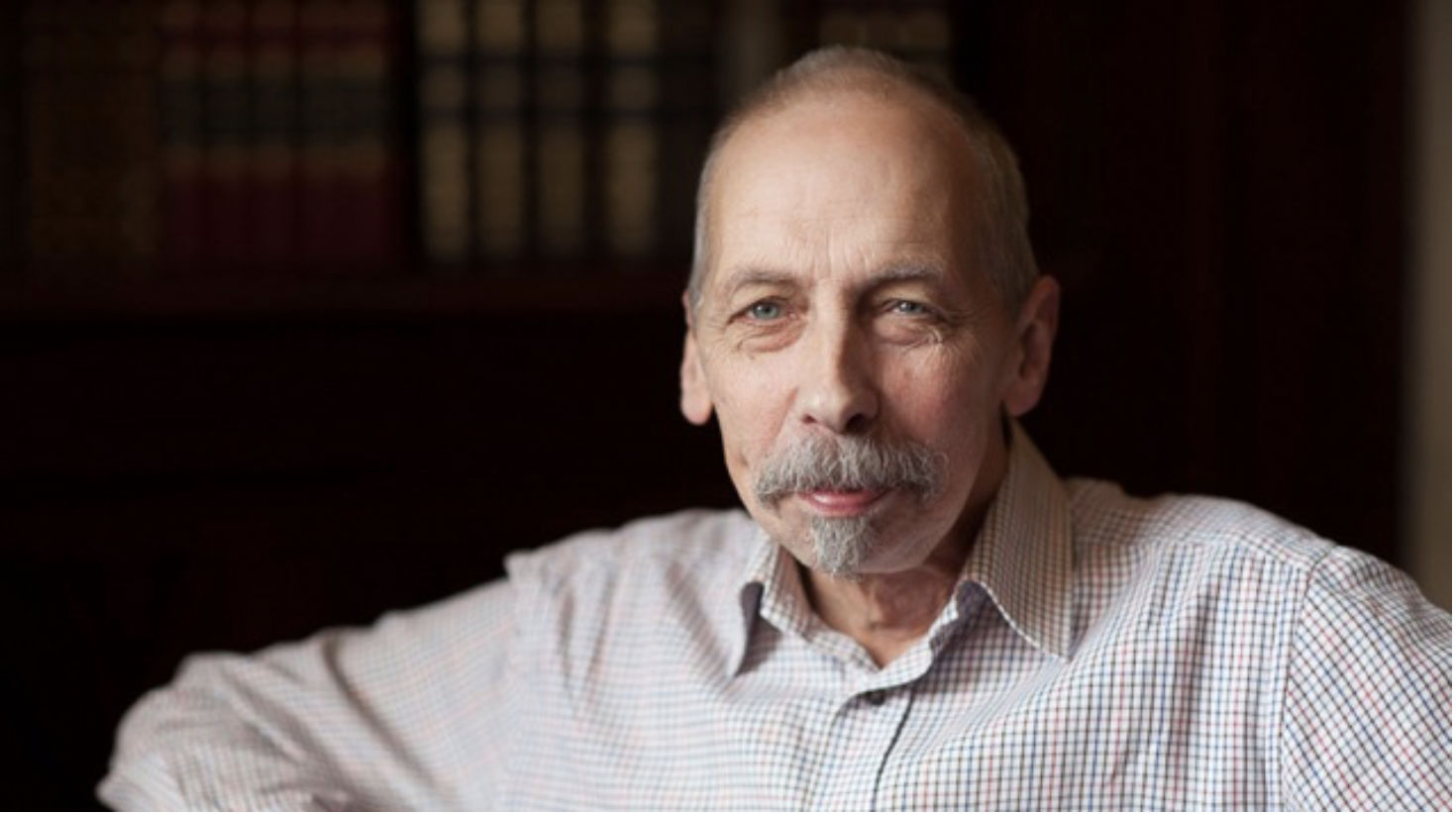
“I am what is often referred to as a patient partner in health and social care research. I bring my direct personal experience to what has been so often a missing voice at the table. Nowadays, I tend to be more of an advocate and advisor for Patient, Public Involvement (PPI) in research.
PPI – Patient, Public Involvement is all about actively involving patients, carers and the public with the aim of improving people’s health. It is making sure that those who are likely to benefit from any treatment that is researched are involved throughout the whole process.
I was successfully treated for cancer of the larynx (due to smoking) in the UK. My consultants were leaders in head and neck cancer research. The best evidenced treatment, at that time, was voice box removal, or a laryngectomy. However, my clinicians looked, not only at this evidence, but also at me, the patient. I was given seven weeks of intensive radiotherapy in 1995, and it clearly worked. I have not smoked since and I am healthier as a result, though my voice is rather rough and throaty.
I attended a meeting in London in 1999 where a senior researcher pointed to the many studies on a table and asked, “How should we tell the public about the research trials we do?” I responded by saying that, “it might be better to involve the patients at the beginning, rather than at the end,” which appeared to be what they wanted to hear. I was subsequently invited to a meeting to discuss how national cancer research groups, those working nationally in cancer research, might form a small group to advise on how patient involvement would work. That’s when my involvement in PPI began.
In Ireland, you have the Health Research Board‘s PPI Ignite Network. The network promotes excellence and inspires innovation in public and patient involvement in health and social care research in Ireland. It enables many people with different conditions, illnesses and experiences, together with smaller and larger charities, to make it better now and in the future.
Our researchers are, simply, quite brilliant people. They often pursue their question late in the evening due to the demands of clinical practice. Too much time is spent seeking funding, completing endless forms and trying to understand, rather than working in a more effective manner. I suppose that my time as a teacher taught me that disruption is good in any system. I saw the opportunities to help with different studies as learning opportunities, where I could expand my knowledge and skills. Creating and building mutual learning are central to meaningful involvement.
The first programme of the HRB-Trials Methodology Research Network (based in University of Galway) identified and prioritised the Top 10 methodology questions on how we ‘recruit’ participants to randomised trials. The next looked at ‘retention’ of participants in trials and the most recent one I worked in was led by Evidence Synthesis Ireland (also based in University of Galway) and looked at priorities in rapid syntheses of evidence to inform policy and practice.
The shift for me was that this was exploring the uncertainties of the research methods that are used and is not relying on my personal experience as a patient. It is about objectively considering what we all don’t know and prioritising questions for research.
Later, I was invited to speak at a conference and to join the conversations about how Ireland’s focus on improving health and well-being was key in involvement making that purposeful difference. When we collaborate to enrich research methods, they have the potential to bring about better and more meaningful research, and better outcomes for patients and the public.